
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea (Diabetes Metab J 2020;44: 699-710)
- Hoon Sung Choi, Sung Woo Lee, Jin Taek Kim, Hong Kyu Lee
- Diabetes Metab J. 2020;44(6):944-945. Published online December 23, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0249
- 3,454 View
- 61 Download
- Metabolic Risk/Epidemiology
- The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea
- Hoon Sung Choi, Sung Woo Lee, Jin Taek Kim, Hong Kyu Lee
- Diabetes Metab J. 2020;44(5):699-710. Published online April 16, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0109
- 6,160 View
- 104 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
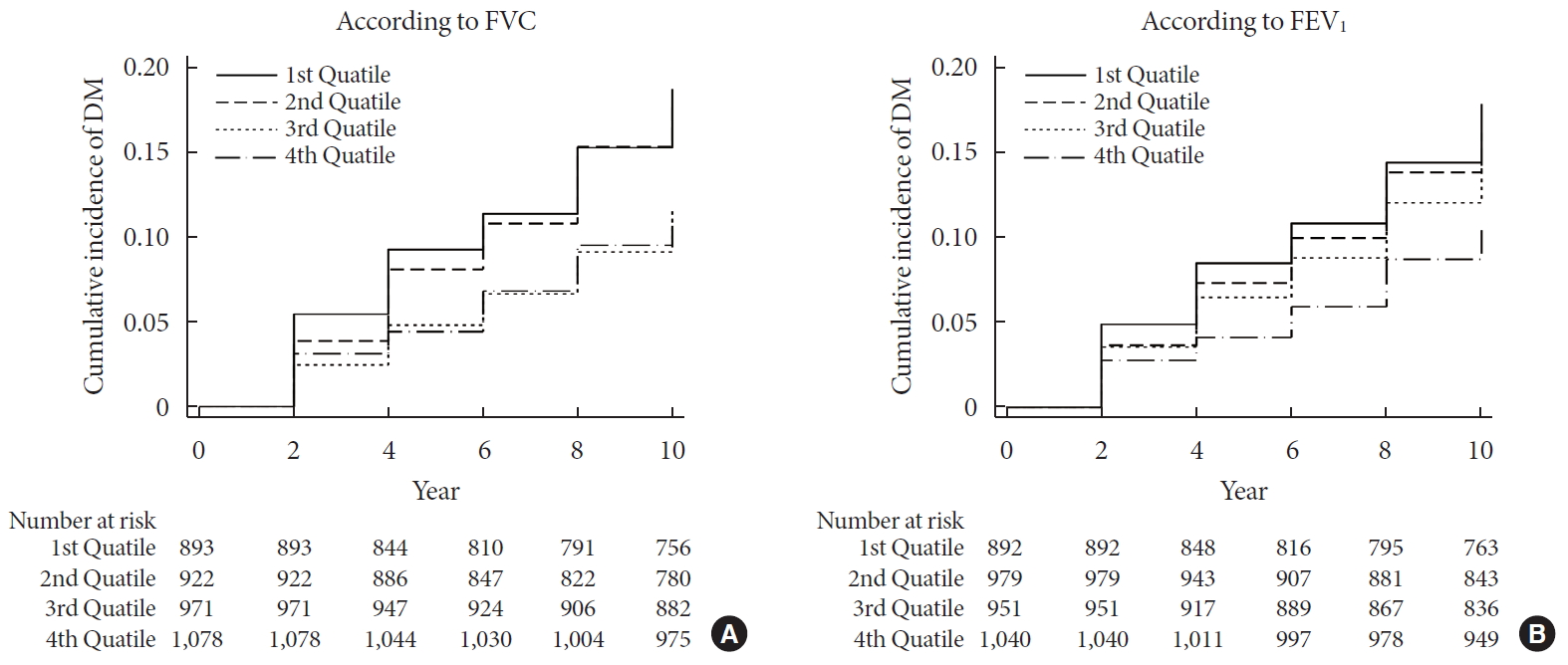
ePub Background We sought to explore whether reduced pulmonary function is an independent risk factor for incident diabetes in Koreans.
Methods We conducted a prospective cohort study of pulmonary function as a risk factor for incident diabetes using 10-year follow-up data from 3,864 middle-aged adults from the Ansung cohort study in Korea. The incidence of diabetes was assessed using both oral glucose tolerance tests and glycosylated hemoglobin levels.
Results During 37,118 person-years of follow-up, 583 participants developed diabetes (incidence rate: 15.7 per 1,000 person-years). The mean follow-up period was 8.0±3.7 years. Forced vital capacity (FVC; % predicted) and forced expiratory volume in 1 second (FEV1; % predicted) were significantly correlated with incident diabetes in a graded manner after adjustment for sex, age, smoking, exercise, and metabolic parameters. The adjusted hazard ratio (HR) and confidence interval (CI) for diabetes were 1.408 (1.106 to 1.792) and 1.469 (1.137 to 1.897) in the first quartiles of FVC and FEV1, respectively, when compared with the highest quartile. Furthermore, the FVC of the lowest first and second quartiles showed a significantly higher 10-year panel homeostasis model assessment of insulin resistance index, with differences of 0.095 (95% CI, 0.010 to 0.018;
P =0.028) and 0.127 (95% CI, 0.044 to 0.210;P =0.003), respectively, when compared to the highest quartiles.Conclusion FVC and FEV1 are independent risk factors for developing diabetes in Koreans. Pulmonary factors are possible risk factors for insulin resistance and diabetes.
-
Citations
Citations to this article as recorded by- Validation of the Framingham Diabetes Risk Model Using Community-Based KoGES Data
Hye Ah Lee, Hyesook Park, Young Sun Hong
Journal of Korean Medical Science.2024;[Epub] CrossRef - Independent and combined associations of multiple-heavy-metal exposure with lung function: a population-based study in US children
Yiting Chen, Anda Zhao, Rong Li, Wenhui Kang, Jinhong Wu, Yong Yin, Shilu Tong, Shenghui Li, Jianyu Chen
Environmental Geochemistry and Health.2023; 45(7): 5213. CrossRef - Role of Pulmonary Function in Predicting New-Onset Cardiometabolic Diseases and Cardiometabolic Multimorbidity
Guochen Li, Yanqiang Lu, Yanan Qiao, Die Hu, Chaofu Ke
Chest.2022; 162(2): 421. CrossRef - Reduced lung function predicts risk of incident type 2 diabetes: insights from a meta-analysis of prospective studies
Yunping Zhou, Fei Meng, Min Wang, Linlin Li, Pengli Yu, Yunxia Jiang
Endocrine Journal.2022; 69(3): 299. CrossRef - Development of Various Diabetes Prediction Models Using Machine Learning Techniques
Juyoung Shin, Jaewon Kim, Chanjung Lee, Joon Young Yoon, Seyeon Kim, Seungjae Song, Hun-Sung Kim
Diabetes & Metabolism Journal.2022; 46(4): 650. CrossRef - Improving Machine Learning Diabetes Prediction Models for the Utmost Clinical Effectiveness
Juyoung Shin, Joonyub Lee, Taehoon Ko, Kanghyuck Lee, Yera Choi, Hun-Sung Kim
Journal of Personalized Medicine.2022; 12(11): 1899. CrossRef - The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea (Diabetes Metab J 2020;44: 699-710)
Hoon Sung Choi, Sung Woo Lee, Jin Taek Kim, Hong Kyu Lee
Diabetes & Metabolism Journal.2020; 44(6): 944. CrossRef - The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea (Diabetes Metab J 2020;44: 699-710)
Jin Hwa Kim
Diabetes & Metabolism Journal.2020; 44(6): 940. CrossRef
- Validation of the Framingham Diabetes Risk Model Using Community-Based KoGES Data
- Fracture Incidence and Risk of Osteoporosis in Female Type 2 Diabetic Patients in Korea
- Jong Kwan Jung, Hyo Jeong Kim, Hong Kyu Lee, Sang Soo Kim, Chan Soo Shin, Jin Taek Kim
- Diabetes Metab J. 2012;36(2):144-150. Published online April 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.2.144
- 4,282 View
- 38 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background There are no published data regarding fracture risk in type 2 diabetic patients in Korea. In this study, we compared the fracture incidence and risk of osteoporosis of type 2 diabetic female patients with those in a non-diabetic hypertensive cohort.
Methods The incidence of fracture in a type 2 diabetic cohort was compared with that in a non-diabetic hypertensive cohort over the course of 7 years. Female type 2 diabetic and non-diabetic hypertensive patients who visited Eulji General Hospital outpatient clinic from January 2004 to April 2004 were assigned to the diabetic cohort and the non-diabetic hypertensive cohort, respectively. Surveys on fracture event, use of anti-osteoporosis medications, and bone mineral density were performed.
Results The number of fractures was 88 in the female diabetic cohort (
n =1,268, 60.6±11.5 years) and 57 in the female non-diabetic hypertensive cohort (n =1,014, 61.4±11.7 years). The RR in the diabetic cohort was 1.38 (P =0.064; 95% confidence interval [CI], 0.98 to 1.94) when adjusted for age. Diabetic patients with microvascular complications (61.0%) showed a higher RR of 1.81 (P =0.014; 95% CI, 1.13 to 2.92) compared with those without these complications. The prevalence of osteoporosis was comparable between the groups, while use of anti-osteoporosis medication was more common in the diabetic cohort (12.8%) than in the hypertensive cohort (4.5%) (P <0.001).Conclusion In our study, a higher fracture risk was observed in female type 2 diabetics with microvascular complications. Special concern for this risk group is warranted.
-
Citations
Citations to this article as recorded by- Research Progress on How to Prevent Osteoporosis in Diabetic Patients
婷玉 牛
Advances in Clinical Medicine.2022; 12(02): 1178. CrossRef - Differences in the roles of types 1 and 2 diabetes in the susceptibility to the risk of fracture: a systematic review and meta-analysis
Jiaqing Dou, Jing Wang, Qiu Zhang
Diabetology & Metabolic Syndrome.2021;[Epub] CrossRef - The risk of hip and non-vertebral fractures in type 1 and type 2 diabetes: A systematic review and meta-analysis update
Tatiane Vilaca, Marian Schini, Susan Harnan, Anthea Sutton, Edith Poku, Isabel E. Allen, Steven R. Cummings, Richard Eastell
Bone.2020; 137: 115457. CrossRef - Diabetes mellitus and risk of low-energy fracture: a meta-analysis
Jing Bai, Qian Gao, Chen Wang, Jia Dai
Aging Clinical and Experimental Research.2020; 32(11): 2173. CrossRef - Diabetes mellitus and the risk of fractures at specific sites: a meta-analysis
Hao Wang, Ying Ba, Qian Xing, Jian-Ling Du
BMJ Open.2019; 9(1): e024067. CrossRef - The use of metformin, insulin, sulphonylureas, and thiazolidinediones and the risk of fracture: Systematic review and meta‐analysis of observational studies
Khemayanto Hidayat, Xuan Du, Meng‐Jiao Wu, Bi‐Min Shi
Obesity Reviews.2019; 20(10): 1494. CrossRef - Bei Diabetikern an eine Osteoporose denken!
Stephan Scharla
MMW - Fortschritte der Medizin.2018; 160(21-22): 65. CrossRef - Type 2 diabetes and risk of low-energy fractures in postmenopausal women: meta-analysis of observational studies
Joanna Dytfeld, Michał Michalak
Aging Clinical and Experimental Research.2017; 29(2): 301. CrossRef - Risk of low-energy fracture in type 2 diabetes patients: a meta-analysis of observational studies
P. Jia, L. Bao, H. Chen, J. Yuan, W. Liu, F. Feng, J. Li, H. Tang
Osteoporosis International.2017; 28(11): 3113. CrossRef - Comorbidity and its relationship with health service use and cost in community-living older adults with diabetes: A population-based study in Ontario, Canada
Kathryn Fisher, Lauren Griffith, Andrea Gruneir, Dilzayn Panjwani, Sima Gandhi, Li (Lisa) Sheng, Amiram Gafni, Patterson Chris, Maureen Markle-Reid, Jenny Ploeg
Diabetes Research and Clinical Practice.2016; 122: 113. CrossRef - Type 2 diabetes mellitus and bone fragility: Special focus on bone imaging
Yong Jun Choi, Yoon-Sok Chung
Osteoporosis and Sarcopenia.2016; 2(1): 20. CrossRef - Epidemiology of fractures in type 2 diabetes
Ann V. Schwartz
Bone.2016; 82: 2. CrossRef - Efficacy and Safety of Weekly Alendronate Plus Vitamin D35600 IU versus Weekly Alendronate Alone in Korean Osteoporotic Women: 16-Week Randomized Trial
Kwang Joon Kim, Yong-Ki Min, Jung-Min Koh, Yoon-Sok Chung, Kyoung Min Kim, Dong-Won Byun, In Joo Kim, Mikyung Kim, Sung-Soo Kim, Kyung Wan Min, Ki Ok Han, Hyoung Moo Park, Chan Soo Shin, Sung Hee Choi, Jong Suk Park, Dong Jin Chung, Ji Oh Mok, Hong Sun Ba
Yonsei Medical Journal.2014; 55(3): 715. CrossRef - Increased Risk of Fracture and Postfracture Adverse Events in Patients With Diabetes: Two Nationwide Population-Based Retrospective Cohort Studies
Chien-Chang Liao, Chao-Shun Lin, Chun-Chuan Shih, Chun-Chieh Yeh, Yi-Cheng Chang, Yuan-Wen Lee, Ta-Liang Chen
Diabetes Care.2014; 37(8): 2246. CrossRef - Aortic Calcification and Bone Metabolism: The Relationship between Aortic Calcification, BMD, Vertebral Fracture, 25-Hydroxyvitamin D, and Osteocalcin
Kwang Joon Kim, Kyoung Min Kim, Kyeong Hye Park, Han Seok Choi, Yumie Rhee, Yong Ho Lee, Bong Soo Cha, Myong Jin Kim, Sun Min Oh, J. Keenan Brown, Sung Kil Lim
Calcified Tissue International.2012; 91(6): 370. CrossRef
- Research Progress on How to Prevent Osteoporosis in Diabetic Patients
- Prevalence and Clinical Characteristics of Recently Diagnosed Type 2 Diabetes Patients with Positive Anti-Glutamic Acid Decarboxylase Antibody
- Yul Hwangbo, Jin Taek Kim, Eun Ky Kim, Ah Reum Khang, Tae Jung Oh, Hak Chul Jang, Kyong Soo Park, Seong Yeon Kim, Hong Kyu Lee, Young Min Cho
- Diabetes Metab J. 2012;36(2):136-143. Published online April 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.2.136
- 4,559 View
- 40 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Latent autoimmune diabetes in adults (LADA) refers to a specific type of diabetes characterized by adult onset, presence of islet auto-antibodies, insulin independence at the time of diagnosis, and rapid decline in β-cell function. The prevalence of LADA among patients with type 2 diabetes varies from 2% to 20% according to the study population. Since most studies on the prevalence of LADA performed in Korea were conducted in patients who had been tested for anti-glutamic acid decarboxylase antibody (GADAb), a selection bias could not be excluded. In this study, we examined the prevalence and clinical characteristics of LADA among adult patients recently diagnosed with type 2 diabetes.
Methods We included 462 patients who were diagnosed with type 2 diabetes within 5 years from the time this study was performed. We measured GADAb, fasting insulin level, fasting C-peptide level, fasting plasma glucose level, HbA1c, and serum lipid profiles and collected data on clinical characteristics.
Results The prevalence of LADA was 4.3% (20/462) among adult patients with newly diagnosed type 2 diabetes. Compared with the GADAb-negative patients, the GADAb-positive patients had lower fasting C-peptide levels (1.2±0.8 ng/mL vs. 2.0±1.2 ng/mL,
P =0.004). Other metabolic features were not significantly different between the two groups.Conclusion The prevalence of LADA is 4.3% among Korean adult patients with recently diagnosed type 2 diabetes. The Korean LADA patients exhibited decreased insulin secretory capacity as reflected by lower C-peptide levels.
-
Citations
Citations to this article as recorded by- The worldwide prevalence of latent autoimmune diabetes of adults among adult-onset diabetic individuals: a systematic review and meta-analysis
Deepika Ramu, Selvaraj Ramaswamy, Suresh Rao, Solomon F. D. Paul
Endocrine.2023; 82(1): 28. CrossRef - Investigation of serum level relationship anti-glutamic acid decarboxylase antibody and inflammatory cytokines (IL1-β, IL-6) with vitamins D in type 2 diabetes
Vahid Pouresmaeil, Sarmad Mashayekhi, Mohammad Sarafraz Yazdi
Journal of Diabetes & Metabolic Disorders.2022; 21(1): 181. CrossRef - Recent information on test utilization and intraindividual change in anti-glutamic acid decarboxylase antibody in Korea: a retrospective study
Rihwa Choi, Wonseo Park, Gayoung Chun, Jiwon Lee, Sang Gon Lee, Eun Hee Lee
BMJ Open Diabetes Research & Care.2022; 10(3): e002739. CrossRef - Prevalence and factors associated with latent autoimmune diabetes in adults (LADA): a cross-sectional study
Anselmo M. Manisha, Aminiel R. Shangali, Sayoki G. Mfinanga, Erasto V. Mbugi
BMC Endocrine Disorders.2022;[Epub] CrossRef - Latent Autoimmune Diabetes in Adults (LADA) and its Metabolic Characteristics among Yemeni Type 2 Diabetes Mellitus Patients
Dhekra Al-Zubairi, Molham AL-Habori, Riyadh Saif-Ali
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 4223. CrossRef - Therapeutic approaches for latent autoimmune diabetes in adults: One size does not fit all
Theocharis Koufakis, Niki Katsiki, Pantelis Zebekakis, George Dimitriadis, Kalliopi Kotsa
Journal of Diabetes.2020; 12(2): 110. CrossRef - Long‐term effects on glycaemic control and β‐cell preservation of early intensive treatment in patients with newly diagnosed type 2 diabetes: A multicentre randomized trial
Suk Chon, Sang Youl Rhee, Kyu Jeung Ahn, Sei Hyun Baik, Yongsoo Park, Moon Suk Nam, Kwan Woo Lee, Soon Jib Yoo, Gwanpyo Koh, Dae Ho Lee, Young Seol Kim, Jeong‐Taek Woo
Diabetes, Obesity and Metabolism.2018; 20(5): 1121. CrossRef - A Global Perspective of Latent Autoimmune Diabetes in Adults
Rajashree Mishra, Kenyaita M. Hodge, Diana L. Cousminer, Richard D. Leslie, Struan F.A. Grant
Trends in Endocrinology & Metabolism.2018; 29(9): 638. CrossRef - The prevalence of latent autoimmune diabetes in adults and its correlates in patients with type 2 diabetes in Kerman, Iran [2011]
Gozashti Mohammad Hossein, Shafiei Maryam, Esmaeilian Saeed, Najafipour Hamid, Mashrouteh Mahdieh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2015; 9(2): 104. CrossRef - Low prevalence of latent autoimmune diabetes in adults in northern India
A. Sachan, G. Zaidi, R. P. Sahu, S. Agrawal, P. G. Colman, E. Bhatia
Diabetic Medicine.2015; 32(6): 810. CrossRef - Amelioration of Diabetes-induced Cognitive Deficits by GSK-3β Inhibition is Attributed to Modulation of Neurotransmitters and Neuroinflammation
Ashok Kumar Datusalia, Shyam Sunder Sharma
Molecular Neurobiology.2014; 50(2): 390. CrossRef - Successful treatment of latent autoimmune diabetes in adults with Traditional Chinese Medicine: a case report
Jiaxing Tian, Wenke Liu, Zhong Zhen, Xiaolin Tong
Journal of Traditional Chinese Medicine.2013; 33(6): 766. CrossRef - Clinical characteristics and insulin independence of Koreans with new‐onset type 2 diabetes presenting with diabetic ketoacidosis
H. Seok, C. H. Jung, S. W. Kim, M. J. Lee, W. J. Lee, J. H. Kim, B‐W. Lee
Diabetes/Metabolism Research and Reviews.2013; 29(6): 507. CrossRef - A Case of Latent Autoimmune Diabetes in Adults Developed after Surgical Cure of Growth Hormone Secreting Pituitary Tumor
Wonjin Kim, Jung Ho Kim, Youngsook Kim, Ji Hye Huh, Su Jin Lee, Mi Sung Park, Eun Yeong Choe, Jeong Kyung Park, Myung Won Lee, Jae Won Hong, Byung Wan Lee, Eun Seok Kang, Bong Soo Cha, Eun Jig Lee, Hyun Chul Lee
Endocrinology and Metabolism.2012; 27(4): 318. CrossRef - Latent Autoimmune Diabetes in Adults: Autoimmune Diabetes in Adults with Slowly Progressive β-cell Failure
Hannah Seok, Byung Wan Lee
Diabetes & Metabolism Journal.2012; 36(2): 116. CrossRef
- The worldwide prevalence of latent autoimmune diabetes of adults among adult-onset diabetic individuals: a systematic review and meta-analysis
- Increasing Trend in the Number of Severe Hypoglycemia Patients in Korea
- Jin Taek Kim, Tae Jung Oh, Ye An Lee, Jun Ho Bae, Hyo Jeong Kim, Hye Seung Jung, Young Min Cho, Kyong Soo Park, Soo Lim, Hak Chul Jang, Hong Kyu Lee
- Diabetes Metab J. 2011;35(2):166-172. Published online April 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.2.166
- 65,535 View
- 66 Download
- 30 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background To investigate whether the number of subjects with severe hypoglycemia who are brought to a hospital emergency department is increasing and to identify whether there have been changes in the demographic and clinical characteristics of those subjects.
Methods We analyzed data from the Emergency Departments of two general hospitals in Seoul, Korea. We included data from all adult subjects with type 2 diabetes who presented to an emergency department with severe hypoglycemia between January 1, 2004 and December 30, 2009.
Results A total of 740 cases of severe hypoglycemia were identified. The mean subject age was 69±12 years, mean duration of diabetes was 13.8±9.3 years, and 53.2% of subjects were receiving insulin therapy. We observed a sharp rise in the number of cases between 2006 and 2007. Stages 3-5 chronic kidney disease was diagnosed in 31.5% of subjects, and low C-peptide levels (<0.6 ng/mL) were found in 25.5%. The mean subject age, duration of diabetes, HbA1c level, and renal and insulin secretory function values did not change significantly during the study period. The proportion of glimepiride use increased, while use of gliclazide decreased among sulfonylurea users. Use of insulin analogues increased, while use of NPH/RI decreased among insulin users.
Conclusion We identified a sharp increase in the number of subjects with severe hypoglycemia presenting to an emergency room since 2006. The clinical characteristics of these subjects did not change markedly during the study period. Nationwide studies are warranted to further clarify this epidemic of severe hypoglycemia.
-
Citations
Citations to this article as recorded by- Hypoglycemia Unawareness—A Review on Pathophysiology and Clinical Implications
Laura Hölzen, Bernd Schultes, Sebastian M. Meyhöfer, Svenja Meyhöfer
Biomedicines.2024; 12(2): 391. CrossRef - Hospital admissions trends for severe hypoglycemia in diabetes patients in Spain, 2005 to 2015
Domingo Orozco-Beltrán, Alberto Guillen-Mollá, Ana María Cebrián-Cuenca, Jorge Navarro-Pérez, Vicente F. Gil-Guillén, Jose A. Quesada, Francisco J. Pomares-Gómez, Adriana Lopez-Pineda, Concepción Carratalá-Munuera
Diabetes Research and Clinical Practice.2021; 171: 108565. CrossRef - Trends and risk factors in severe hypoglycemia among individuals with type 2 diabetes in Korea
Seung Eun Lee, Kyoung-Ah Kim, Kang Ju Son, Sun Ok Song, Kyeong Hye Park, Se Hee Park, Joo Young Nam
Diabetes Research and Clinical Practice.2021; 178: 108946. CrossRef - Predisposing factors of hypoglycemia in patients with type 2 diabetes mellitus presented with symptomatic hypoglycemia in a tertiary hospital of Bangladesh
AjitK Paul, A.B.M. Kamrul-Hasan
Journal of Diabetology.2020; 11(3): 163. CrossRef - Real-world risk of hypoglycemia-related hospitalization in Japanese patients with type 2 diabetes using SGLT2 inhibitors: a nationwide cohort study
Takeshi Horii, Yoichi Oikawa, Narumi Kunisada, Akira Shimada, Koichiro Atsuda
BMJ Open Diabetes Research & Care.2020; 8(2): e001856. CrossRef - Association between BMI and risk of severe hypoglycaemia in type 2 diabetes
J.-S. Yun, Y.-M. Park, K. Han, S.-A. Cha, Y.-B. Ahn, S.-H. Ko
Diabetes & Metabolism.2019; 45(1): 19. CrossRef - The effects of hypoglycaemia and dementia on cardiovascular events, falls and fractures and all‐cause mortality in older individuals: A retrospective cohort study
Katharina Mattishent, Kathryn Richardson, Ketan Dhatariya, George M. Savva, Chris Fox, Yoon K. Loke
Diabetes, Obesity and Metabolism.2019; 21(9): 2076. CrossRef - Detection of asymptomatic drug-induced hypoglycemia using continuous glucose monitoring in older people – Systematic review
K. Mattishent, Y.K. Loke
Journal of Diabetes and its Complications.2018; 32(8): 805. CrossRef - Incidence rate and patient characteristics of severe hypoglycemia in treated type 2 diabetes mellitus patients in Japan: Retrospective Diagnosis Procedure Combination database analysis
Yuika Ikeda, Takekazu Kubo, Eisei Oda, Machiko Abe, Shigeru Tokita
Journal of Diabetes Investigation.2018; 9(4): 925. CrossRef - A study to evaluate the prevalence of impaired awareness of hypoglycaemia in adults with type 2 diabetes in outpatient clinic in a tertiary care centre in Singapore
Ling Zhu, Li Chang Ang, Wee Boon Tan, Xiaohui Xin, Yong Mong Bee, Su-Yen Goh, Ming Ming Teh
Therapeutic Advances in Endocrinology and Metabolism.2017; 8(5): 69. CrossRef - Baseline-Corrected QT (QTc) Interval Is Associated with Prolongation of QTc during Severe Hypoglycemia in Patients with Type 2 Diabetes Mellitus
Seon-Ah Cha, Jae-Seung Yun, Tae-Seok Lim, Yoon-Goo Kang, Kang-Min Lee, Ki-Ho Song, Ki-Dong Yoo, Yong-Moon Park, Seung-Hyun Ko, Yu-Bae Ahn
Diabetes & Metabolism Journal.2016; 40(6): 463. CrossRef - Response: Cardiovascular Disease Predicts Severe Hypoglycemia in Patients with Type 2 Diabetes (Diabetes Metab J 2015;39:498-506)
Jae-Seung Yun, Yu-Bae Ahn
Diabetes & Metabolism Journal.2016; 40(1): 85. CrossRef - 1,5-Anhydro-D-Glucitol Could Reflect Hypoglycemia Risk in Patients with Type 2 Diabetes Receiving Insulin Therapy
Min Kyeong Kim, Hye Seung Jung, Soo Heon Kwak, Young Min Cho, Kyong Soo Park, Seong Yeon Kim
Endocrinology and Metabolism.2016; 31(2): 284. CrossRef - Severe Hypoglycemia and Cardiovascular or All-Cause Mortality in Patients with Type 2 Diabetes
Seon-Ah Cha, Jae-Seung Yun, Tae-Seok Lim, Seawon Hwang, Eun-Jung Yim, Ki-Ho Song, Ki-Dong Yoo, Yong-Moon Park, Yu-Bae Ahn, Seung-Hyun Ko
Diabetes & Metabolism Journal.2016; 40(3): 202. CrossRef - Hypoglycemia and Health Costs
Yong-ho Lee, Gyuri Kim, Eun Seok Kang
The Journal of Korean Diabetes.2016; 17(1): 11. CrossRef - Bi‐directional interaction between hypoglycaemia and cognitive impairment in elderly patients treated with glucose‐lowering agents: a systematic review and meta‐analysis
K. Mattishent, Y. K. Loke
Diabetes, Obesity and Metabolism.2016; 18(2): 135. CrossRef - Trend of antihyperglycaemic therapy and glycaemic control in 184,864 adults with type 1 or 2 diabetes between 2002 and 2014: Analysis of real-life data from the DPV registry from Germany and Austria
Barbara Bohn, Wolfgang Kerner, Jochen Seufert, Hans-Peter Kempe, Peter M. Jehle, Frank Best, Martin Füchtenbusch, Andreas Knauerhase, Martin Hofer, Joachim Rosenbauer, Reinhard W. Holl
Diabetes Research and Clinical Practice.2016; 115: 31. CrossRef - Characteristics of Hypoglycemia Pateints Visiting the Emergency Department of a University Hospital
Sang-Hyeon Choi, Deok-Ki Youn, Moon-Gi Choi, Ohk-Hyun Ryu
The Journal of Korean Diabetes.2016; 17(3): 202. CrossRef - Increasing trend in emergency department visits for hypoglycemia from patients with type 2 diabetes mellitus in Taiwan
Ying-Ju Chen, Chen-Chang Yang, Lynn-Chu Huang, Likwang Chen, Chii-Min Hwu
Primary Care Diabetes.2015; 9(6): 490. CrossRef - Intensive Individualized Reinforcement Education Is Important for the Prevention of Hypoglycemia in Patients with Type 2 Diabetes
Yun-Mi Yong, Kyung-Mi Shin, Kang-Min Lee, Jae-Young Cho, Sun-Hye Ko, Min-Hyang Yoon, Tae-Won Kim, Jong-Hyun Jeong, Yong-Moon Park, Seung-Hyun Ko, Yu-Bae Ahn
Diabetes & Metabolism Journal.2015; 39(2): 154. CrossRef - 1,5-Anhydroglucitol as a Useful Marker for Assessing Short-Term Glycemic Excursions in Type 1 Diabetes
Hannah Seok, Ji Hye Huh, Hyun Min Kim, Byung-Wan Lee, Eun Seok Kang, Hyun Chul Lee, Bong Soo Cha
Diabetes & Metabolism Journal.2015; 39(2): 164. CrossRef - A nationwide population-based study on the risk of coma, ketoacidosis and hypoglycemia in patients with celiac disease and type 1 diabetes
Matthew Kurien, Kaziwe Mollazadegan, David S. Sanders, Jonas F. Ludvigsson
Acta Diabetologica.2015; 52(6): 1167. CrossRef - Blood electrolyte disturbances during severe hypoglycemia in Korean patients with type 2 diabetes
Mi Yeon Kang
The Korean Journal of Internal Medicine.2015; 30(5): 648. CrossRef - Cardiovascular Disease Predicts Severe Hypoglycemia in Patients with Type 2 Diabetes
Jae-Seung Yun, Seung-Hyun Ko, Sun-Hye Ko, Ki-Ho Song, Ki-Dong Yoo, Kun-Ho Yoon, Yong-Moon Park, Yu-Bae Ahn
Diabetes & Metabolism Journal.2015; 39(6): 498. CrossRef - The Influence of Admission Hypoglycemia on Clinical Outcomes in Acute Myocardial Infarction Patients with Diabetes Mellitus
Eun Jung Kim, Myung Ho Jeong, In Seok Jeong, Sang Gi Oh, Sang Hyung Kim, Young keun Ahn, Ju Han Kim, Young Jo Kim, Shung Chull Chae, Taek Jong Hong, In Whan Seong, Jei Keon Chae, Chong Jin Kim, Myeong Chan Cho, Ki Bae Seung, Hyo Soo Kim
Korean Journal of Medicine.2014; 87(5): 565. CrossRef - Corrected QT Interval Prolongation during Severe Hypoglycemia without Hypokalemia in Patients with Type 2 Diabetes
Jae Won Beom, Jung Min Kim, Eun Joo Chung, Ju Yeong Kim, Seung Yeong Ko, Sang Don Na, Cheol Hwan Kim, Gun Park, Mi Yeon Kang
Diabetes & Metabolism Journal.2013; 37(3): 190. CrossRef - Presence of Macroalbuminuria Predicts Severe Hypoglycemia in Patients With Type 2 Diabetes
Jae-Seung Yun, Sun-Hye Ko, Sun-Hee Ko, Ki-Ho Song, Yu-Bae Ahn, Kun-Ho Yoon, Yong-Moon Park, Seung-Hyun Ko
Diabetes Care.2013; 36(5): 1283. CrossRef - Severe Hypoglycemia in Patients with Diabetes
Jae Seung Yun, Seung-Hyun Ko
Diabetes & Metabolism Journal.2012; 36(4): 273. CrossRef - Severe hypoglycaemia requiring the assistance of emergency medical services - frequency, causes and symptoms
Veronika Krnacova, Ales Kubena, Karel Macek, Martin Bezdek, Alena Smahelova, Jiri Vlcek
Biomedical Papers.2012; 156(3): 271. CrossRef - Higher Morning to Evening Ratio in Total Dose of Twice-Daily Biphasic Insulin Analog Might Be Effective in Achieving Glucose Control in Patients with Poorly Controlled Type 2 Diabetes
Yong-Ho Lee, Byung-Wan Lee, Hea Jin Kwon, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee
Diabetes Technology & Therapeutics.2012; 14(6): 508. CrossRef
- Hypoglycemia Unawareness—A Review on Pathophysiology and Clinical Implications
- Association Between Volume of Bowls and the Dietary Intakes in Subjects with Type 2 Diabetes.
- Hee Jung Ahn, Bo Kyung Koo, Ji Yeon Jung, Hwi Ryun Kwon, Mi Yeon Chung, Yun Hyi Ku, Jin Taek Kim, Kyung Ah Han, Kyung Wan Min
- Korean Diabetes J. 2009;33(4):335-343. Published online August 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.4.335
- 2,569 View
- 24 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The results of previous studies suggest that portion size is a major factor dictating dietary energy intake. We investigated the relationship between frequencies of rice meals, bowl volumes, and dietary energy intake in a sample of patients with type 2 diabetes. METHODS: A total of 203 type 2 diabetes patients were enrolled in the study. A one-week food diary was collected from each patient and used to assess the types of meal consumed as well as the context of consumption. The volumes of the eating vessels (rice, soup and side dish bowls) used by each patient were obtained by comparisons to measuring cylinders, and dietary energy and macronutrient intake were estimated for each patient by consulting three-day dietary records. RESULTS: The mean age of the 203 subjects (male: 76, female: 127) was 53.9 +/- 9.1 years and the average body mass index (BMI) was 25.6 +/- 4.2 kg/m2. Among the subjects who ate three times per day, 96.4% consumed rice more than twice out of three meals. The median volume of rice bowls used by patients was 350 cc, of soup bowls was 530 cc and of side dish bowls was 260 cc. Portion size, as estimated by rice bowl volume, was not associated with BMI. Male subjects tended to eat out of larger rice and soup bowls (P < 0.001). Portion size was correlated with energy intake from rice (P = 0.021), but not with total energy intake (kcal/kg/day), especially in male subjects. CONCLUSION: Portion size of rice bowl was correlated with energy intake from rice, but not with total energy intake in male subjects with type 2 diabetes. To design effective meal planning methods for patients with type 2 diabetes, further prospective studies are warranted to investigate causative relationships between portion size andmetabolic conditions as well as variation by gender. -
Citations
Citations to this article as recorded by- Trends in adherence to dietary recommendations among Korean type 2 diabetes mellitus patients
Kyong Park
Nutrition Research and Practice.2015; 9(6): 658. CrossRef - Small Rice Bowl-Based Meal Plan for Energy and Marcronutrient Intake in Korean Men with Type 2 Diabetes: A Pilot Study
Hee Jung Ahn, Kyung Ah Han, Jin Young Jang, Jae Hyuk Lee, Kang Seo Park, Kyung Wan Min
Diabetes & Metabolism Journal.2011; 35(3): 273. CrossRef - Nutrients and Dish Intake by Fasting Blood Glucose Level
Jihyun Choi, Hyun-Kyung Moon
The Korean Journal of Nutrition.2010; 43(5): 463. CrossRef - Small Rice Bowl-Based Meal Plan versus Food Exchange-Based Meal Plan for Weight, Glucose and Lipid Control in Obese Type 2 Diabetic Patients
Hee-Jung Ahn, Kyung-Ah Han, Hwi-Ryun Kwon, Bo-Kyung Koo, Hyun-Jin Kim, Kang-Seo Park, Kyung-Wan Min
Korean Diabetes Journal.2010; 34(2): 86. CrossRef - The Effects of Small Sized Rice Bowl on Carbohydrate Intake and Dietary Patterns in Women with Type 2 Diabetes
Hee-Jung Ahn, Yu-Kyung Eom, Kyung-Ah Han, Hwi-Ryun Kwon, Hyun Jin Kim, Kang Seo Park, Kyung-Wan Min
Korean Diabetes Journal.2010; 34(3): 166. CrossRef - The Small Rice Bowl-Based Meal Plan was Effective at Reducing Dietary Energy Intake, Body Weight, and Blood Glucose Levels in Korean Women with Type 2 Diabetes Mellitus
Hee Jung Ahn, Kyung Ah Han, Hwi Ryun Kwon, Kyung Wan Min
Korean Diabetes Journal.2010; 34(6): 340. CrossRef
- Trends in adherence to dietary recommendations among Korean type 2 diabetes mellitus patients

 KDA
KDA
 First
First Prev
Prev





